When Coders don’t agree, who is correct? The Physician office? The Hospital Facility?
by Lori-Lynne A. Webb, CPC, CCS-P, CCP, CHDA, COBGC, CDIP
Coding can be a challenge when coders are confronted with procedures that are new, and include changes to traditional clinical concepts of coding and patient care. This can problematic when evaluating an addition to the procedure code, or using guidelines from specialty physician groups who have come forth with new clinical guidelines and/or techniques to be used when performing surgery. Many times, these specialty resources for physicians include recommendations for coding/billing of new surgical procedures and guidelines. Hospital based facility coders traditionally use only an encoder, and are not normally exposed to or educated in the specialty based areas, when these changes take place.
Tubal Ligation via Salpingectomy – ACOG speaks
In regard to the “accepted” clinical standard, ACOG published the ACOG committee opinion #620 in January 2015, in their eyes, ovarian cancer may originate in the fallopian tube leading to a new standard of care, At this time they are pursuing more research, but agreed that if a patient was in for a tubal ligation, to excize the entire tube rather than only a portion of the tube for elective sterilization. This is now considered a tubal ligation via salpingectomy.
Unfortunately, for coders; there is no CPT code for this idea of reporting a prophylactic salpingectomy at athe time of tubal ligation. CPT gives us a code for “salpingectomy” or “tubal ligation” ACOG has given the physicians/surgeons coding options for this type or clinical care and reporting.
In querying ACOG as to how should reporting/coding be done, they have stated that salpingectomy code 58700 should NEVER be used to report a sterilization procedure of any sort. The rationale behind this is that the RVU values of the salpingectomy code include the pathological changes and additional risk included in those changes that cause complications such as blocked tubes, adhesions, or even benign or neoplastic effects. Their recommendation for coding is you code as per the “intent” of doing a tubal ligation. In the request of clarity and transparency in coding and documentation, on the “notes” line of your claim form you should include a brief statement “tubal ligation via salpingectomy”.
Issue: Facility codes as “Salpingectomy”; Physician codes as “Tubal Ligation”
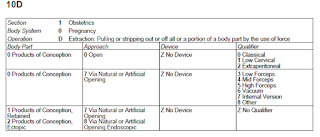
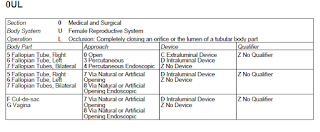
The issue has come up that when hospital inpatient coders code for a “tubal ligation via salpingectomy” we are seeing these coded via the encoder as a standard salpingectomy – and the diagnosis appended to the facility claim is till sterilization. This is problematic as you can see below”
1) The physician’s billing and the facility billing do not match (cpt codes)
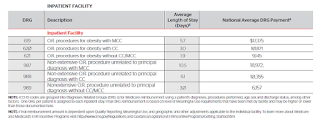
2) The facility has been reimbursed at a higher RVU value rate for a salpingectomy than what is reimbursed for a traditional tubal ligation
3) The physician and/or facility may be denied payment by a third party payer (insurance carrier) due to the claims do not ‘match’.
4) The patient ends up with a large “bill” from the non-payment of either the physician billing or the hospital/facility billing due to this mis-match on the claims.
5) The facility claims they have coded correctly – as they do not recognize ACOG specialty guidelines for billing of facility charges for OB and GYN services.
… And we have very complicated issues….
When this issue came up, the physician office was informed by the facility that they had “coded the procedure” incorrectly, and to immediately file a corrected claim showing “salpingectomy” instead of “Tubal ligation” as the facility had not been paid.
The physician office countered this inquiry back to the facility; stating they were following the coding direction of ACOG and the clinical rationale behind performing salpingectomy vs/tubal ligation, and also the reimbursement rationale of why the physician should not be entitled to a higher reimbursement RVU value for this service.
As you can see below, the RV values are significantly higher for the traditional salpingectomy than for the tubal ligation(s). Also, the edits, show the salpingectomy is subject to 10 post op/ follow up days, and the tubal ligation(s) are subject to 90 post op follow up days. This will also impact how care is delivered to the patient post surgery.
 (Salpingectomy)
(Salpingectomy)  (Tubal Ligations)
(Tubal Ligations) The facility coder then stated that when they ran the scenario through the encoder, it directed them to code the salpingectomy. Unfortunately, the encoder does not take into consideration the “reason” for the salpingectomy was for contraception (elective) not medically indicated (eg disease of the tube). In addition the facility stated that CPT, also does not have a variance, or guideline for coding the “tubal ligation” code when a “salpingectomy” is performed.
Both sides of this issue have valid reasons for coding the way they did. Unfortunately, the facility has not been paid, and has turned this billing over to patient responsibility. Both side of this issue feel that the coding was coded correctly. However, all coders should also adhere to the AHIMA and/or AAPC standards of ethical conduct when coding.
1. Apply accurate, complete, and consistent coding practices for the production of high-quality healthcare data.
2. Report all healthcare data elements (e.g. diagnosis and procedure codes, present on admission indicator, discharge status) required for external reporting purposes (e.g. reimbursement and other administrative uses, population health, quality and patient safety measurement, and research) completely and accurately, in accordance with regulatory and documentation standards and requirements and applicable official coding conventions, rules, and guidelines.
3. Assign and report only the codes and data that are clearly and consistently supported by health record documentation in accordance with applicable code set and abstraction conventions, rules, and guidelines.
4. Query provider (physician or other qualified healthcare practitioner) for clarification and additional documentation prior to code assignment when there is conflicting, incomplete, or ambiguous information in the health record regarding a significant reportable condition or procedure or other reportable data element dependent on health record documentation (e.g. present on admission indicator).
5. Refuse to change reported codes or the narratives of codes so that meanings are misrepresented.
6. Refuse to participate in or support coding or documentation practices intended to inappropriately increase payment, qualify for insurance policy coverage, or skew data by means that do not comply with federal and state statutes, regulations and official rules and guidelines.
7. Facilitate interdisciplinary collaboration in situations supporting proper coding practices.
8. Advance coding knowledge and practice through continuing education.
9. Refuse to participate in or conceal unethical coding or abstraction practices or procedures.
10. Protect the confidentiality of the health record at all times and refuse to access protected health information not required for coding-related activities ( examples of coding-related activities include completion of code assignment, other health record data abstraction, coding audits, and educational purposes).
11. Demonstrate behavior that reflects integrity, shows a commitment to ethical and legal coding practices, and fosters trust in professional activities.
AAPC Code of Ethics (Link to AAPC ethics documents)
It shall be the responsibility of every AAPC member, as a condition of continued membership, to conduct themselves in all professional activities in a manner consistent with ALL of the following ethical principles of professional conduct:
- Integrity
- Respect
- Commitment
- Competence
- Fairness
- Responsibility
Adherence to these ethical standards assists in assuring public confidence in the integrity and professionalism of AAPC members. Failure to conform professional conduct to these ethical standards, as determined by AAPC's Ethics Committee, may result in the loss of membership with AAPC.
AAPC and its Ethics Committee does not function as a judiciary body. Any complaint to AAPC should have a foundation in law (for example, someone has been found guilty of fraud or has been placed on the Medicare Exclusion List) or a foundation in AAPC administrative rules (for example, counterfeit CEUs or a member using credentials falsely
AAPC and its Ethics Committee does not function as a judiciary body. Any complaint to AAPC should have a foundation in law (for example, someone has been found guilty of fraud or has been placed on the Medicare Exclusion List) or a foundation in AAPC administrative rules (for example, counterfeit CEUs or a member using credentials falsely
Resolution?
The resolution for this case was for the facility to send an appeal back to the 3rd party carrier showing the rationale for each side of the issue. (Eg; why the physician/surgeon/provider coded as a “tubal ligation via salpingectomy” and the facility rationale for how the “computerized encoder” directed the facility to code as a traditional salpingectomy)
At this time, the burden of payment now lies squarely on the 3rd party insurance payer. While this is not a perfect solution, it clearly shows that a resolution can be had, but both the physician provider and the facility have a vital stake in needing reimbursement, yet have completely different ideas as to what is “right” and “wrong” with how this should be coded.
In the ever-changing world of medicine, these situations are becoming more and more common. New tools are being developed for usage in operative procedures, new clinical information is now being discovered via scientific medical research. CPT procedures, ICD10 pcs, and encoders all struggle with maintaining the database and guidelines for each, based upon these clinical and scientific developments for appropriate patient care.
In regard to the contraceptive vs/medically indicated issue; many third party payers do not pay for contraceptive procedures, but they do pay for medically necessary procedures (such as a salpingectomy) when there is a diagnostic reason. In these cases, it is best to contact the 3rdparty payer/insurancecarrier in advance to verify what coverage the patient may have. . If coverage is not available or uncertain, be prepared to have the patient sign an advanced beneficiary notice and/or request payment in full at the time services are rendered.
It is also advisable to contact and communicate with the facility to inform them of your “anticipated” coding prior to a surgery/procedure being performed. All parties should be informed of the intent and “pre-authorize/pre-code” for the procedure. These should include
a) Physician Office, coder, biller, and physician
b) Facility/Hospital coder, and encoder manager
c) Patient
d) Third party insurance payer/pre-authorization
In conclusion, the above scenario is not the only surgical scenario that this may happen with. This can happen when a physician may perform what they deem as “medically necessary” and the facility deem as “cosmetic”.. so communication becomes a critical issue in these cases. Resolution for these types of issues take perseverance and the willingness to understand the coding rationale on both sides to come to a good overall solution for all parties involved.
Editor’s note: Lori-Lynne A. Webb, CPC, CCS-P, CCP, CHDA, CDIP, COBGC and ICD10 cm/pcs Ambassador/trainer is an E&M, and Procedure based Coding, Compliance, Data Charge entry and HIPAA Privacy specialist, with over 20 years of experience. Lori-Lynne’s coding specialty is OB/GYN office & Hospitalist Services, Maternal Fetal Medicine, OB/GYN Oncology, Urology, and general surgical coding. She can be reached via e-mail at webbservices.lori@gmail.com or you can also find current coding information on her blog site: http://lori-lynnescodingcoachblog.blogspot.com/.